The Basics
Depersonalization/Derealization disorder (DDD) is a dissociative condition, characterised by feelings of detachment from the self and others.
Research indicates that on average 50% of the global population will experience some form of dissociation at least once in their lifetime. However, chronic or recurrent symptoms affect only 1% to 2% of the general population.
Common symptoms include:
Distorted, “dreamy” or “foggy” perception of the self and the surrounding world;
Altered perception of time;
You might feel detached, void of feelings, like a robot;
You might have difficulty recognizing yourself in the mirror and recall memories that feel emotionally distant.
The causes of Depersonalization/Derealization disorder are still poorly understood, although some of the most common include:
A traumatic experience, like being the victim of a crime or a car accident;
Following the use of illicit substances;
Increased anxiety, stress or fear;
Childhood abuse.
The most commonly used instrument for diagnosing DDD worldwide is the Cambridge Depersonalization Scale or CDS, developed by Sierra and Berrios in the year 2000.
This scale has 29 questions, inquiring about feelings the respondent might be experiencing. The scale assesses the frequency of such symptoms and their approximate duration.

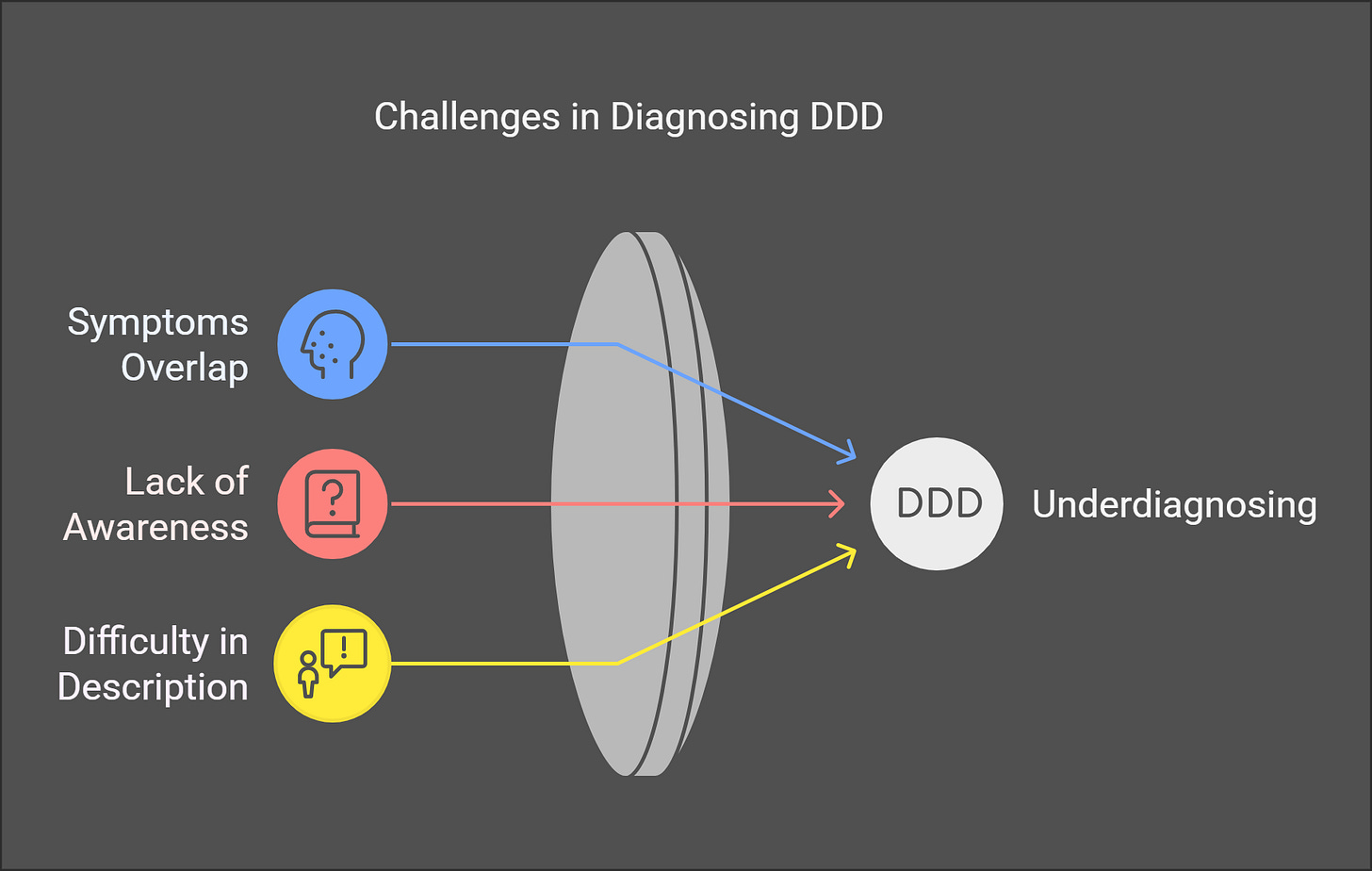
Depersonalization/Derealization is often underdiagnosed for multiple reasons, the most common being:
Some symptoms of DDD overlap with other psychiatric conditions further complicating the diagnostic process; (Source)
It appears that many mental health professionals lack fundamental knowledge about the condition and therefore might struggle to identify it; (Source)
Some of the symptoms of DDD are very hard to describe, particularly those related to dissociation and a “foggy” or “dreamy” vision. (Source)
Technical Bits
The Term
Historically, the oldest evidence of clinical patients suffering from Depersonalization/Derealization dates back to the middle of the 19th century in France, where multiple physicians reported patients with symptoms consistent with DDD.
The term was coined by the French psychologist Ludovic Dugas, who encountered the condition while studying déjà vu in 1894 and borrowed the term from the Swiss philosopher Henri-Frédéric Amiel.
Overlapping Symptoms
One of the most complex aspects of identifying and diagnosing Depersonalization/Derealization is that some of its symptoms do indeed overlap with those of other conditions. Leading some mental health professionals to focus on the most common ones and end up ignoring the presence of Depersonalization/Derealization.
Here is a breakdown of the most common feelings, sensations, and symptoms that characterise DDD and how they are shared with other conditions:
Brain Functions and Neurology
The brain mechanisms of Depersonalization/Derealization disorder are still poorly understood and theories on the matter are sometimes contradicting.
Some researchers believe that dissociation and emotional numbing in DDD might be some defence mechanisms that are developed to help the mind detach and protect itself from unavoidable trauma or stress.
Another neurobiological model suggests that DDD involves prefrontal cortical inhibition of the amygdala and anterior cingulate cortex, resulting in heightened alertness coupled with a dampened emotional processing or “numbing”. This model provides a potential explanation for the paradoxical combination of experiencing contrasting sensations of hypervigilance or “reality checks” and emotional detachment.
Neuroimaging studies of DDD have identified specific patterns of brain activity associated with the condition, including increased left frontal-temporal activation and decreased left caudate perfusion (Hollander et al., 1992).
These findings draw parallels to the neurobiological profile of obsessive-compulsive disorder or “OCD”, suggesting a potential shared mechanism and highlighting the need for further research in this field.
Another study conducted a PET study exploring differences in brain activities between DDD patients and healthy controls. It discovered decreased metabolic activity in the right temporal regions, like Brodmann’s areas 22 and 21, and increased activity in parietal areas 7B and 39 and left occipital area 19. The study found that activity in the 7B parietal area might dictate symptom severity.
Treatments
To this day, Depersonalization/Derealization Disorder does not have a “standardised treatment”. What does this mean?
That the treatment you will be offered will depend on the knowledge and opinion of the mental health professionals you encounter.
For example, it is common practice nearly worldwide to prescribe psychotherapy and antidepressants for individuals affected by depression, this is a “standardised treatment”. For DDD there is no such thing, yet.
But regardless of this, over the last half-century, multiple studies investigated possible treatments for DDD, including:
Cognitive Behavioural Therapy (CBT)
Despite the fancy name, CBT is a widespread form of talking therapy, which attempts to understand and change eventual negative thoughts and behaviours to feel better and to cope with difficulties more effectively.
Multiple studies found CBT to reduce symptoms of DDD:
McRedmond et al., 2024
Pharmacological Approaches
Premise: Remember, no medication is universally effective for mental health conditions. Clinical studies have shown partial efficacy for the following treatments, but individual responses may vary.
Multiple studies over the years explored the effectiveness of pharmacological approaches in treating DDD, the ones that found the best results are:
Selective Serotonin Reuptake Inhibitor or SSRIs: Halder et al., 2023, M. Sierra, 2008, Hollander et al., 1990.
Lamotrigine: Medford et al., 2018, Somer et al., 2013.
Although several studies have explored the effects of various medications on DDD, further research with larger clinical samples is urgently required to enhance our understanding.
Dance therapy
New approaches have looked at Dance Therapy or Dance Movement Therapy (DMT) for the treatment of DDD.
DMT emerged in the 1940s in the United States; a therapeutic approach that utilises movement and body expressions to help individuals improve emotional regulation, body awareness and psychological well-being.
Recent studies have suggested that it might provide a symptom reduction in the treatment of DDD.
Important: Please always discuss treatment options with your doctor before deciding on your health.
Essential Readings For A Deeper Understanding
A Case Of 223 Patients With DDD
Depersonalization: A New Look At A Neglected Syndrome (BOOK)